The new technique, known as photometric stereo endoscopy, can capture topographical images of the colon surface along with traditional two-dimensional images. Such images make it easier to see precancerous growths, including flatter lesions that traditional endoscopy usually misses, says Nicholas Durr, a research fellow in the Madrid-MIT M+Vision Consortium, a recently formed community of medical researchers in Boston and Madrid.
“In conventional colonoscopy screening, you look for these characteristic large polyps that grow into the lumen of the colon, which are relatively easy to see,” Durr says. “However, a lot of studies in the last few years have shown that more subtle, nonpolypoid lesions can also cause cancer.”
Durr is the senior author of a paper describing the new technology in the Journal of Biomedical Optics. Lead author of the paper is Vicente Parot, a research fellow in the M+Vision Consortium. Researchers from Massachusetts General Hospital (MGH) also participated in the project.
In the United States, colonoscopies are recommended beginning at age 50, and are credited with reducing the risk of death from colorectal cancer by about half. Traditional colonoscopy uses endoscopes with fiber-optic cameras to capture images.
Durr and his colleagues, seeking medical problems that could be solved with new optical technology, realized that there was a need to detect lesions that colonoscopy can miss. A technique called chromoendoscopy, in which a dye is sprayed in the colon to highlight topographical changes, offers better sensitivity but is not routinely used because it takes too long.
“Photometric stereo endoscopy can potentially provide similar contrast to chromoendoscopy,” Durr says. “And because it’s an all-optical technique, it can give the contrast at the push of a button.”
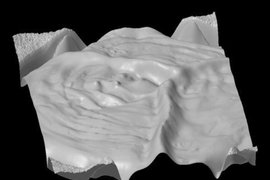
Originally developed as a computer vision technique, photometric stereo imaging can reproduce the topography of a surface by measuring the distances between multiple light sources and the surface. Those distances are used to calculate the slope of the surface relative to the light source, generating a representation of any bumps or other surface features.
However, the researchers had to modify the original technology for endoscopy because there is no way to know the precise distance between the tip of the endoscope and the surface of the colon. Because of this, the images generated during their first attempts contained distortions, particularly in locations where the surface height changes gradually.
To eliminate those distortions, the researchers developed a way to filter out spatial information from the smoothest surfaces. The resulting technology, which requires at least three light sources, does not calculate the exact height or depth of surface features but creates a visual representation that allows the colonoscopist to determine if there is a lesion or polyp.
“What is attractive about this technique for colonoscopy is that it provides an added dimension of diagnostic information, particularly about three-dimensional morphology on the surface of the colon,” says Nimmi Ramanujam, a professor of biological engineering at Duke University who was not part of the research team.
The researchers built two prototypes — one 35 millimeters in diameter, which would be too large to use for colonoscopy, and one 14 millimeters in diameter, the size of a typical colonoscope. In tests with an artificial silicon colon, the researchers found that both prototypes could create 3-D representations of polyps and flatter lesions.
The new technology should be easily incorporated into newer endoscopes, Durr says. “A lot of existing colonoscopes already have multiple light sources,” he says. “From a hardware perspective all they need to do is alternate the lights and then update their software to process this photometric data.”
The researchers plan to test the technology in human patients in clinical trials at MGH and the Hospital Clinico San Carlos in Madrid. They are also working on additional computer algorithms that could help to automate the process of identifying polyps and lesions from the topographical information generated by the new system.
The research was funded by the Comunidad de Madrid through the Madrid-MIT M+Vision Consortium.